What’s the difference between rapid and PCR Covid-19 tests?
A photo comparing a PCR and rapid Covid-19 test
With winter surges, a contagious new variant, and holiday gatherings, Covid-19 testing has been essential. Even before returning to campus, all students were required to get either a negative PCR or rapid test. But what’s the difference between the two?
PCR tests require a trip to a testing site and need a lab to process the results, which come back in a few days. On the other hand, rapid tests are, well, rapid. You can buy them at the store, and results come back in a few minutes. However, there is a higher risk of getting a false negative. So how do these tests work, and why does it make them so different?
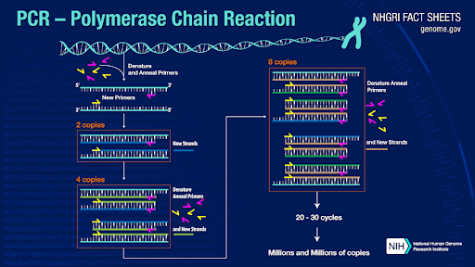
PCR tests use polymerase chain reactions, which amplify genetic material, to detect viral or bacterial infections. A modified version of this PCR, the quantitative polymerase chain reaction (qPCR), is used in order to identify a Covid-19 infection. This modified version adds fluorescent dye in order to measure the amount of genetic material in the sample.
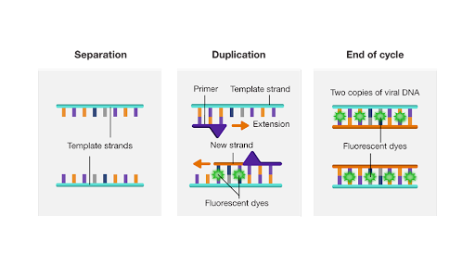
The SARS-CoV-2 virus that causes Covid-19 uses RNA as its genetic material. In the qPCR, through reverse transcription, this RNA is converted into DNA, which is heated until it separates into two strands. SARS-CoV-2 primers attached to the strands ensure that only viral DNA is duplicated. Then, bases attach to the two template strands to form two copies of the viral DNA. The fluorescent dye attaches to the viral DNA, and the process repeats until millions of copies are formed. The successful amplification indicates a positive result.
If the result were negative, the SARS-CoV-2 primers would not match the sample’s genetic material, so there would be no amplification. These PCR tests are the gold standard in diagnosing Covid-19 infections because they can amplify small amounts of viral RNA in order to correctly identify an infection. However, the convenience factor of the rapid test remains unmatched. But why is the rapid test less sensitive than a PCR?
Rapid tests are generally antigen tests, which detect antigens, or molecules on a pathogen’s surface that cause the immune system to produce antibodies. To diagnose Covid-19, the tests look for a protein of the SARS-CoV-2 virus by seeing if it reacts to a solution. These antigen tests do not amplify the viral sample, which is why they are not as sensitive as PCR tests.
If the tests do not detect enough antigens, they may produce a false negative. Antigen tests are more accurate when there is a higher viral load, meaning that if you have symptoms of Covid-19, a rapid antigen test will most likely produce an accurate result. False negatives are more common in the asymptomatic because of the lack of amplification of a low viral load.
So if you have symptoms of Covid-19, a rapid test will probably be accurate. According to experts, you should assume you have Covid-19 if you get a positive rapid result. A negative result is less definitive, and many suggest getting a PCR to confirm it. Because of its amplification, the PCR remains the most accurate for diagnosing Covid-19.
by Hana Shinzawa ’24, Science Editor
24hshinzawa@montroseschool.org